Urinary bladder tumors and bladder cancer, the fourth most common type of cancer in men, are malign tumors originating from the tissues of bladder wall. Its symptoms include frequent urination, sense of burning while urinating, bleeding, incontinence and sudden urge to urinate. In some types of bladder cancer, only treatment is the removal of the bladder. If the bladder should be removed, patients usually delay that surgery and the reason is the necessity of urinary bag use. However, if they know that urinary bag will not be necessary, then they decide for surgery earlier, increasing the likelihood of full recovery. Artificial bladder formed by reshaping the intestines is a method that allows patients to urinate normally and have a more comfortable life. The most important advantage is that this a socially acceptable method that does not lower quality of life. Prof. Dr. Karadeniz explained the treatment of bladder cancer.
What are the causes of bladder cancer?
Bladder is a sphere-like organ that sores the urine coming from both kidneys through urinary tracts (urethra). Malign tumors originating from the inner side of this organ is called bladder cancer. Bladder cancer is more common in men than women. Smoking and chemical substance exposure observed in some factories are among its known causes.
What are the symptoms?
The most important symptom is blood and clots in the urine without pain. In addition, depending on the type of the cancer, complaints like persistent pain during urination and sense of burning towards the end of urination are also reported. This bleeding may not be visible sometimes, but it will be detected in the urine analysis.
How is it diagnosed?
Usually, a mass in the bladder can be easily diagnosed with abdominal or urinary system ultrasonography, and upper and lower Computed Tomography with contrast agent can be used
for diagnosis as well. However, when these examinations are unable to provide a definitive diagnosis, that a method involving the insertion of a camera system through urinary meatus in order to visualize inside the bladder can be used. After diagnosis, Closed TUR Tm (Trans Urethral Resection Tm) operation is performed with an endoscopic camera.
How is TUR Tm performed?
Operation can be performed under general or local anesthesia. Bladder is accessed through urinary meatus and the cancerous section is completely removed and samples are collected from all layers of the bladder by using a special electrical device. The patient can stand up the next day, urinary catheter is generally removed on second or third day and the patient can be discharged.
When is radical cystectomy required?
In this operation; bladder, prostate, portion of the lower urinary tract, seminal vesicles, and lymph nodes around the major surrounding vessels are removed. It takes for 6-8 when performed fully, patient is taken to intensive care for at least 24 hours if needed, and then transferred to the ward. Patients can return home 10-14 days after the operation.
Why the removal of lymph nodes and its number is important?
This is probably the most important part of radical cystectomy operation. Removal of lymph nodes requires special training and experience. However, the more lymph nodes removed the longer the life expectancy of the patient. And in case of cancer in lymphatic tissues, than the actual progression of the disease can be determined for proper planning of additional chemotherapy.
How do patients urinate after the bladder is removed?
The most frequent method is called “ileal conduit”. Both urinary tracts (urethra) are connected to one end of 12-15 cm portion of small intestines and the other end of the intestines is attached to outer abdominal wall. Urine coming to this intestine part via urethra fills into a bag adhered to the skin and the bag is drained by the patients. The urinary bag should be replaced in every 2-3 days. This is artificial bladder (neobladder) method called “orthopedic bladder” which is an important alternative to the old method.
What are the advantages of forming a bladder with intestines?
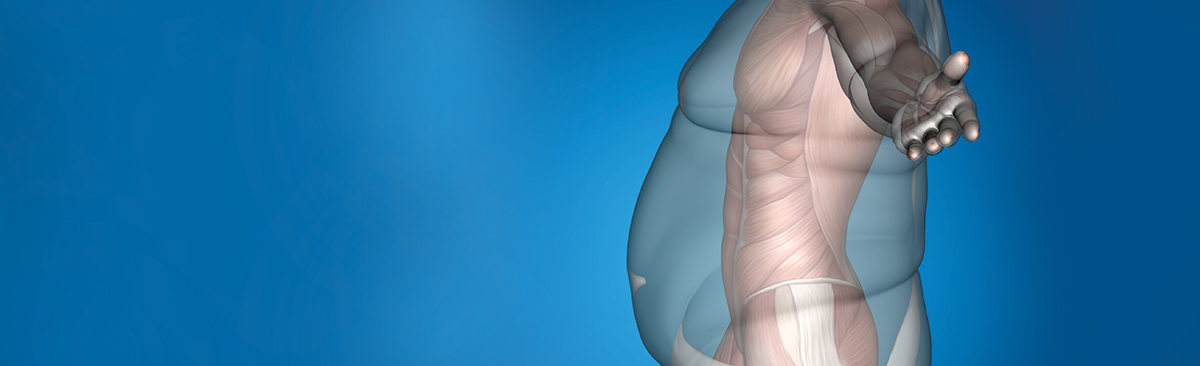
If the removal of bladder is required, it is not easy for patients to make the decision and such delay negatively impact their life. The most important advantage of artificial bladder (neobladder) is that “it does not lower quality of life” and
it is “socially acceptable”. This operation is performed to allow patients to urinate normally in order for them to have a more comfortable life. A portion of the small intestines is reshaped into a sphere and both urinary tracts coming from the kidney are attached to this; one end of this new bladder is then connected to the urinary tract inside the penis. 15-18 days after the operation, the urinary catheter is removed and patients are trained to urinate with their new bladder. Learning to urinate usually takes 4-5 days, and at the end of this period patients become able to fully empty their bladder.